Quick Links
3 easy steps to begin your URAC accreditation
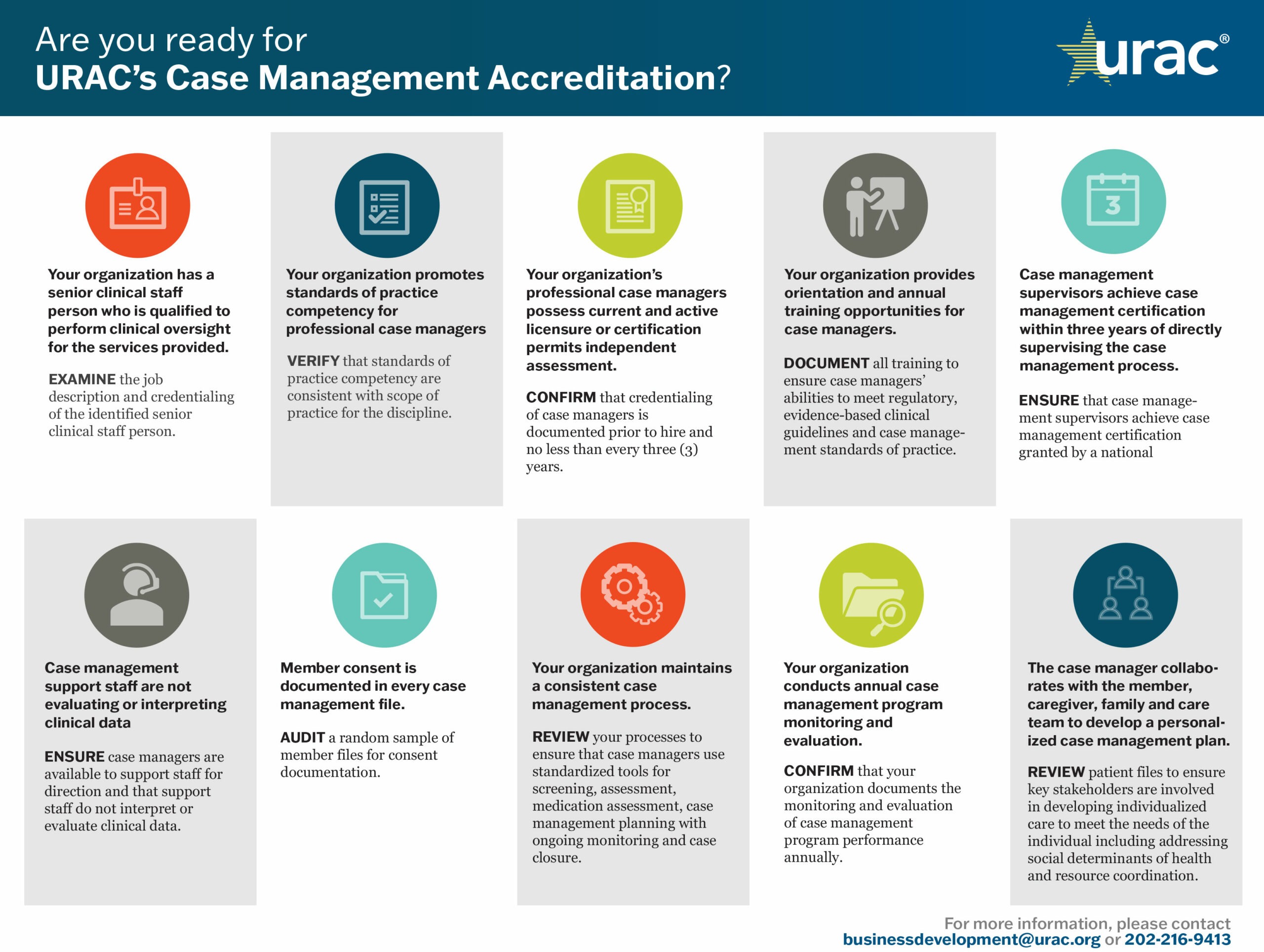
Are you ready?
Download our one page Are You Ready guides for the roadmap to accreditation.
Overview
URAC’s Case Management Accreditation standards and performance measures address the increasing demand for excellence in care coordination, including improved patient engagement, service access and utilization and transitions of care. Understanding the intrinsic value of integrated care, URAC also includes behavioral health components into our case management standards.
Health plans, payers, employers and government agencies recognize URAC Case Management Accreditation as a key catalyst in advancing collaborative care and patient advocacy, particularly for patients transitioning from inpatient care settings. Important to both private and public employers, URAC Case Management Accreditation also authenticates your Disability or Workers’ Compensation case management process to appropriately assess employee readiness for returning to work.
Benefits of Accreditation
By obtaining URAC accreditation, you distinguish your organizational leadership and accountability among other care management programs as well as your commitment to deliver high-quality coordinated care. Additional benefits of Case Management Accreditation include:
- The ability to enhance patient satisfaction through an immersive experience that includes key stakeholders in patient care—consumers and their families, caregivers, providers and non-clinical staff
- Validation of your approach to improve health outcomes by predicting health-related behaviors, applying evidence-based, patient-centric goals and interventions and supporting self-care competencies
- Implementation of risk management oversight and review protocols that reduce client liabilities, enhance data security and ensure regulatory compliance
- Development of a blueprint for ongoing process and quality improvements that enhance care delivery and optimize operational efficiencies
What URAC Standards Address
URAC’s Case Management accreditation standards require companies to establish the policies, procedures and structure needed for optimal performance across four main principles of case management: care coordination, transitions of care, patient engagement and advocacy.
Within six months or less, we will work with your team to understand URAC's standards and flexible framework for continuous improvement. While our experts define the standards of excellence for case management, they do not prescribe how organizations must meet those standards. URAC’s thorough approach stimulates innovation across the continuum of care through email, conference calls and educational webinars.
We award Case Management accreditation for a full three years and we require annual reporting of five quality measures. Download our Case Management Standards-at-a-Glance and Measures-at-a-Glance for more information.
Who May Apply
- This program is for organizations that provide case management services but not for individual case management professionals.
- Organizations that offer a case management program such as hospitals, accountable care organizations, health plans, provider-based practices, clinics and more are welcome to apply for Case Management Accreditation.