Quick Links
Overview
Studies show that convenience, insurance coverage and affordability matter most to people when selecting health care providers and facilities. As patients become more sophisticated consumers of health care—with the help of digital resources—provider experience, reputation and satisfaction ratings/reviews are equally important to them as they navigate the delivery system.
These factors also influence payers such as health plans and hospitals trying to attract and retain health care consumers.
By earning Health Network Accreditation from URAC, you eliminate the guesswork. URAC’s well-respected stamp of approval tells patients and payers that your network meets the highest industry standards in delivering quality care and services.
The URAC Difference
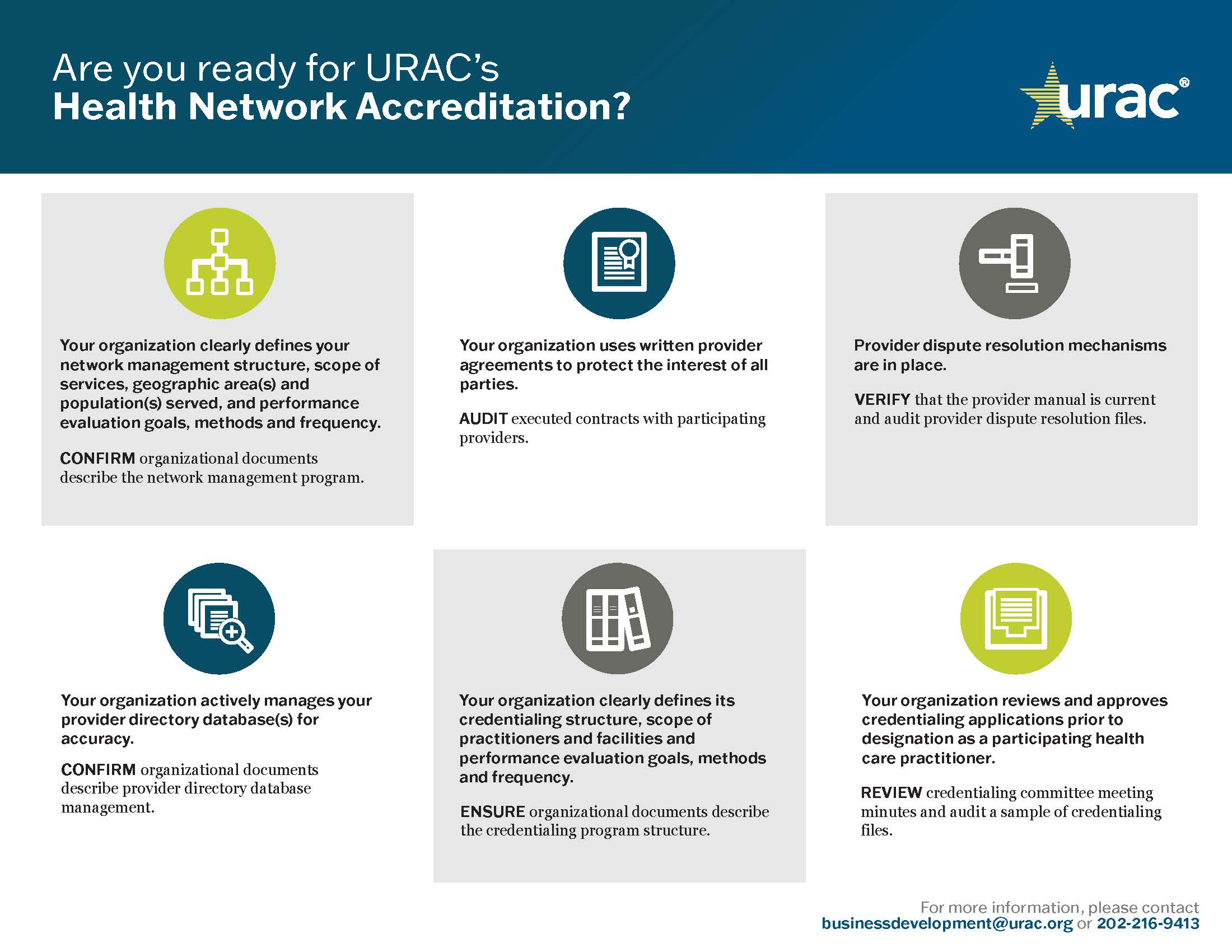
URAC’s Health Network Accreditation standards include key quality benchmarks for network management, provider credentialing and recredentialing, quality management and consumer protections. We also require health networks to establish self-monitoring practices, emphasizing quality assurance and improvement.
The Health Network Accreditation infrastructure requires that you meet for best in class network operations across the following areas:
- Regulatory Compliance
- Operations and Infrastructure
- Performance Monitoring and Improvement
- Consumer Protection and Empowerment
- Information Management
- Network Management
- Credentialing
Benefits of Accreditation
URAC Accreditation assures patients and purchasers that your network providers and facilities meet professional qualifications and have been properly vetted through a rigorous credentialing process. Furthermore, Health Network Accreditation indicates that you continuously monitor and evaluate provider performance, taking quality of care, program compliance and patient feedback into consideration to determine ongoing network participation.
Additional benefits of Health Network Accreditation include:
- Establishment of appropriate patient protections, including formal policies and procedures for confidentiality, complaints, dispute resolution, consumer safety investigations and other issues
- Validation of compliance and adherence to applicable state and federal regulations
- Implementation of risk management oversight and review protocols that prevent, protect and manage client liabilities as well as data security
- Development of a roadmap for ongoing process and quality improvements that enhance care delivery, ensure sound provider practices and optimize operational efficiencies
What to Expect
Within six months or less, we will conduct an independent assessment of your health network. While our experts define the standards of excellence, they do not prescribe how your organization must meet those standards, which provide a flexible framework for continuous improvement.
URAC’s thorough approach stimulates innovation across the continuum of care through email, conference calls and educational webinars.
We award accreditation for a full three years. Review our Health Network Standards-at-a-Glance for more information.
Who May Apply
Preferred provider organizations, provider-based models, behavioral health networks, specialty medical networks (radiologists, audiologists, physical therapists, optometrists, long-term care providers, etc.), physician-hospital organizations, chiropractic networks and workers' compensation networks providers may apply.
Other Administrative Management Accreditation Programs
Health Care Management Certification
Operates in health care and is not eligible for other URAC accreditation
Independent Medical Examination Accreditation
Performs and/or delegates an independent, objective assessment of a patient's medical condition
Health Network Accreditation
Performs and/or delegates health network functions, including management, credentialing and recredentialing