Quick Links
3 easy steps to begin your URAC accreditation
What Our Clients Say...

"Yes, Piedmont was accredited by a different organization in the past. The switch from the other organization to URAC was seamless."
URAC Health Plan Accreditation
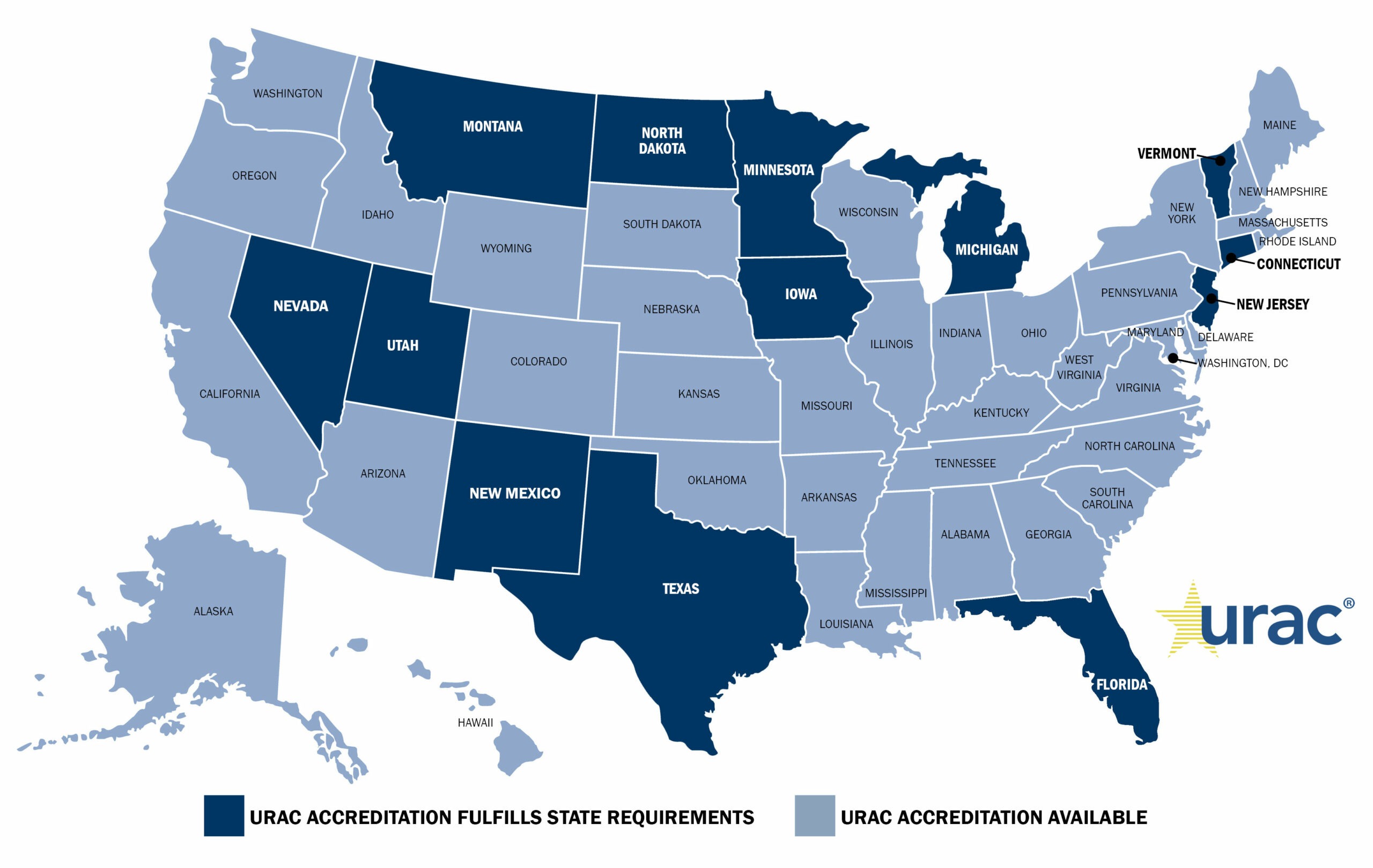
You have a choice in your Health Plan Accreditor!
 Now more than ever, it’s important for health plans of all sizes to ensure they are working with the best accreditor for their needs. URAC’s updated Health Plan Accreditation program addresses the needs of health plans by streamlining our standards to shorten the timeline.
Now more than ever, it’s important for health plans of all sizes to ensure they are working with the best accreditor for their needs. URAC’s updated Health Plan Accreditation program addresses the needs of health plans by streamlining our standards to shorten the timeline.
Our new affordable and competitive pricing ensures health plans get the best value for their accreditation dollars with URAC.
What makes us better than and different from other health plan accreditors? URAC Health Plan Accreditation:
- Allows health plans to be in the driver’s seat to establish their own metrics and performance monitoring so they are meaningful to the plan’s goals.
- Includes contemporary concepts about artificial intelligence, machine learning and regulatory requirements regarding network management.
- Addresses mental health parity, which is increasingly important and enforced by individual states and the Federal Department of Labor.
Long-Term Services and Support (LTSS)
A new, optional Long-Term Services and Supports Module is available for organizations that want to demonstrate their expertise in the broad range of services provided to those with long-term care needs.

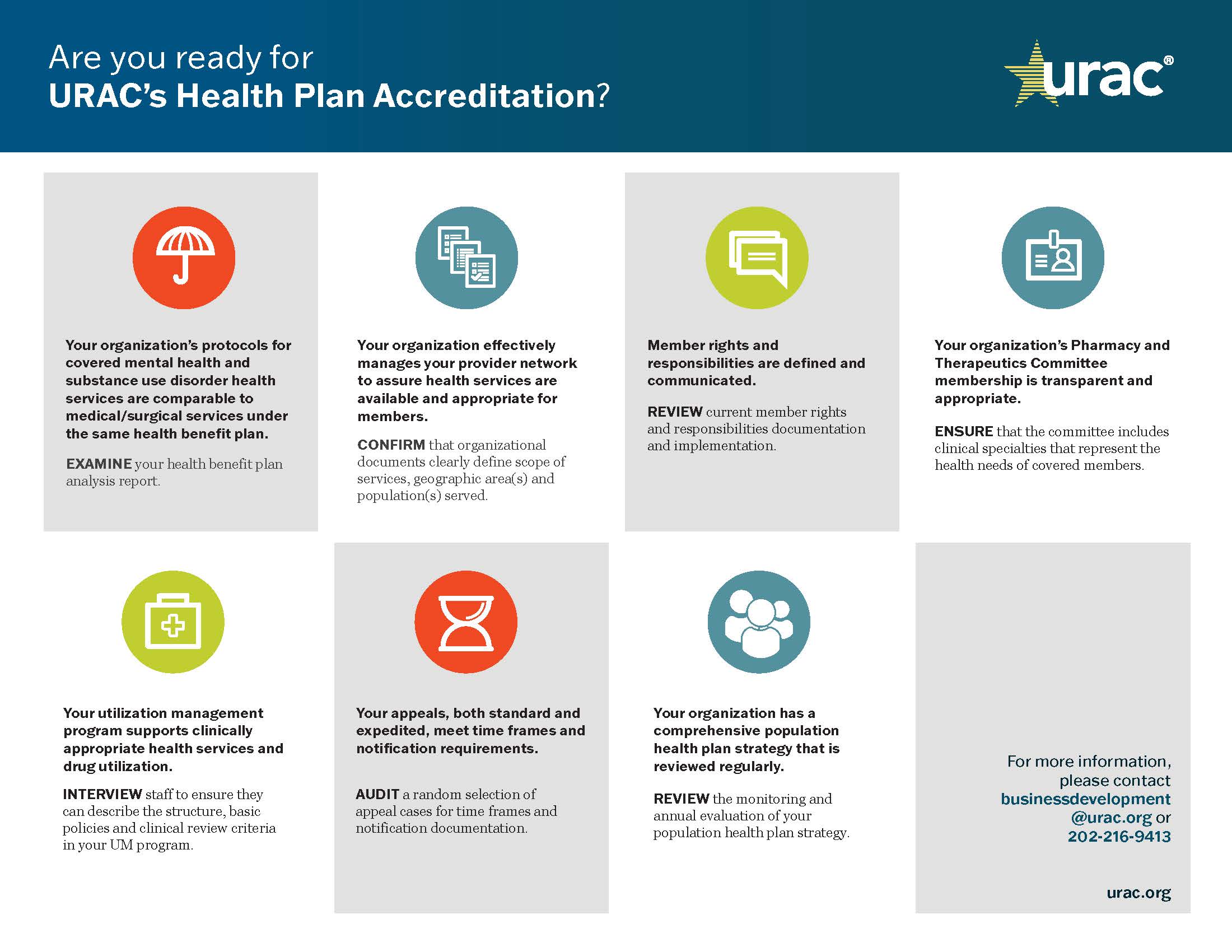
Be Better Prepared
At URAC, our Health Plan Accreditation process is more than collecting metrics and checking boxes. Only URAC offers your health plan a collaborative, comprehensive learning experience, driven by your organization's specific needs.
What does it take to get Accredited
Who May Apply
Health plans, including commercial plans such as health maintenance organizations, preferred provider organization, self-insured and Medicaid plans, are eligible to apply. As a non-profit working to strengthen quality standards across the health care continuum, URAC now offers special pricing to accommodate small health plans.